- HOME
- For Patients
- Glioma
- Treatment of glioma
Glioma
- About glioma
- Symptom of glioma
- Diagnosis of glioma
- Treatment of glioma
- Surgical treatment under the MRI
Treatment of glioma
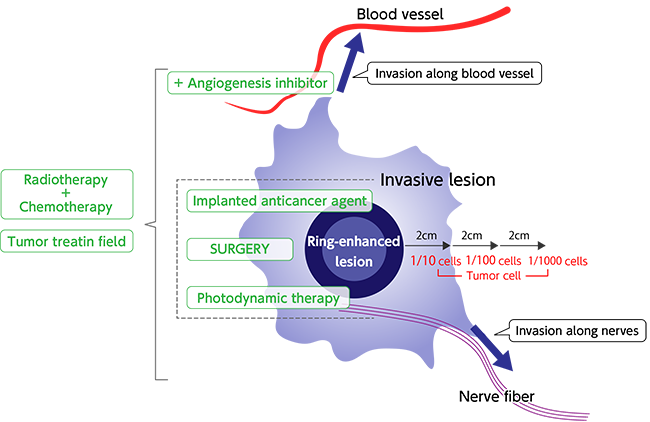
Gliomas are treated with a combination of surgery, radiation therapy, and chemotherapy. Surgery is the basis for all treatments, because it is used not only to determine the type of tumor, but it is the most effective means of removing as much of the tumor as possible. However, distinguishing the border between gliomas and healthy brain tissue is difficult, which means, that in almost all cases, the entire tumor cannot be removed (Figure). At the same time, with advanced-stage tumors, there is a strong correlation between the amount of tumor removed and survival period. Therefore, as much of the tumor as possible needs to be removed.
Tokai University Hospital is one of a small number of institutions in the world where brain tumor surgery is performed using intraoperative MRI so that the surgery can be performed reliably and safely. The hospital also uses an image navigation system and tumor fluorescent labelling (vital staining of tumors) during surgery for removing tumors one by one. However, these surgeries are not simply amatter of removing as much of the tumor as possible; tumor removal also must not damage essential nerve function. Glioma surgery at Tokai University Hospital follows the policy of “removing as much tumor tissue as possible without leaving serious neurological damage.” To achieve this, electroencephalographic examinations and other tests are used during surgery, and in some cases, surgery is even performed while talking with the patient during the operation to confirm language function. Tokai University Hospital has introduced surgical methods in which MRI can be used during surgery, resulting in removal of about 10% more of tumors. Survival times have increased accordingly.
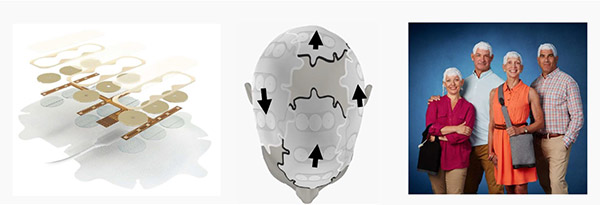
Unfortunately, it is often the case that, even after surgically removing as much of the tumor as feasible, undetected residual glioma is still present. That remaining tumor is treated with radiation therapy and chemotherapy. In recent standard therapy, combination therapy is performed for advanced stage gliomas, starting with radiation therapy for six weeks (radiation once a day, five times a week), and then chemotherapy with an oral anticancer drug (sometimes an intravenous infusion) called Temodar, or temozolomide, that inhibits mitosis (cell division) in tumor cells. Radiation therapy is done with a method in which a somewhat large area is first irradiated, after which radiation is focused on areas that are particularly affected (partial brain radiotherapy) (Figure). Depending on the case, an angiogenesis inhibitor (Avastin) may be used to improve symptoms and delay progression and recurrence. Glioblastoma is the type of glioma with the worst outlook, and when it is diagnosed, the hospital also uses a novel, minimally-invasive treatment called a home tumor treating field system (an electric field is created by electrodes attached to the scalp, which inhibits tumor cell division) that contributes to improving the trajectory ofpatients’ disease. However, because these are tumors associated with a short mean survival time, we do our utmost to match the best treatment toeach individual for a good balance with the patient’s quality of life.
Our intraoperative MRI system was recently upgraded to enhance its performance.

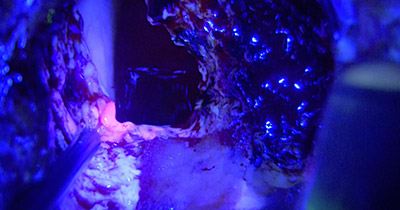
Intraoperative fluorescence diagnosis: Areas colored pink are remaining lesions.
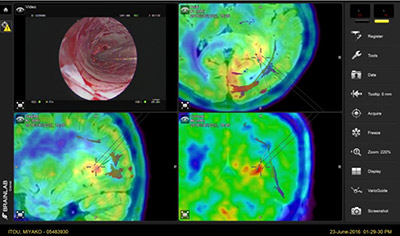
Intraoperative navigation system that uses methionine PET: Visualization of active lesions.
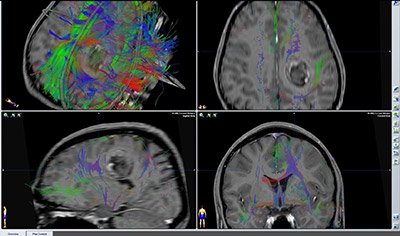
Intraoperative tractography: Visualization of nerve fibers that should be preserved.
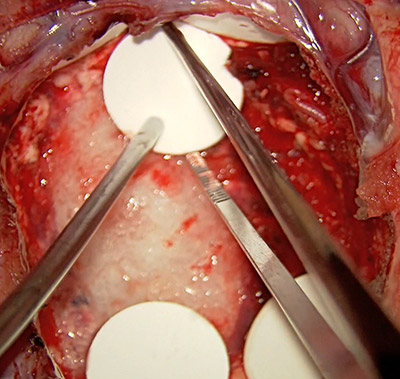
Chemotherapy wafer (Gliadel): Implanted in the extraction cavity with the aim of preventing local recurrence.
Home-use tumor treating field system(Optune®): Treatment is considered according to the circumstances.
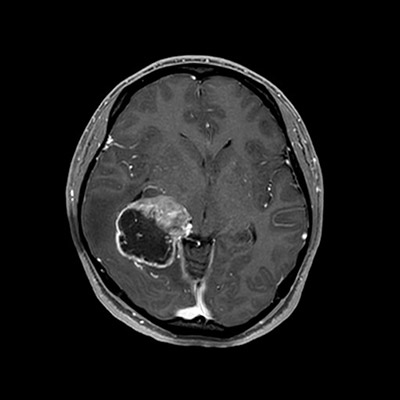
Preoperative MRI
Strong cerebral edema and central structure variation (cerebral herniation) are seen; a lesion suspected of being a malignant tumor with abundant circulation in the center of the lesion is seen.
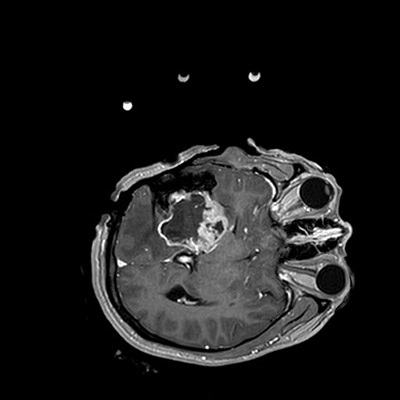
1st intraoperative MRI
Intraoperative MRI is done after decompression for error correction with an intraoperative navigation system due to swelling of the brain after craniotomy caused by cerebral edema.
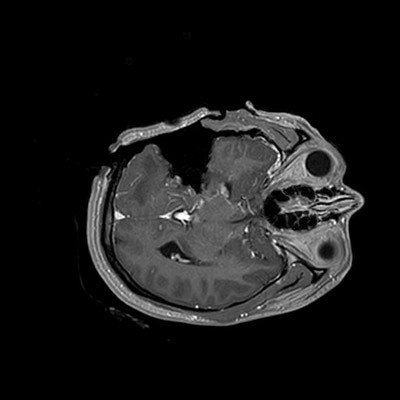
2nd intraoperative MRI
Total removal is confirmed. Confirmation during surgery of whether there is cerebral infarction or hemorrhage is also possible.
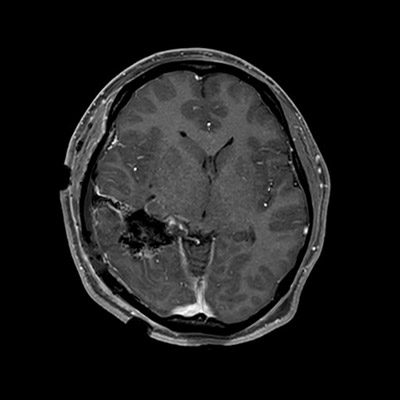
Postoperative day 1 MRI
No postoperative bleeding or cerebral infarction is seen, total removal is achieved, and the course is stable with no sequelae.
Glioma is “Absolute non‐excision.”
Glioblastomas, which have the poorest prognosis, show ring-like contrast enhancement as a result of the tumor vessels that have grown, reflecting the abundant cell division on contrast-enhanced MRI. Even at a distance of 6 cm from the enhanced area, tumor cells are said to exist with a probability of 1/1,000 cells.
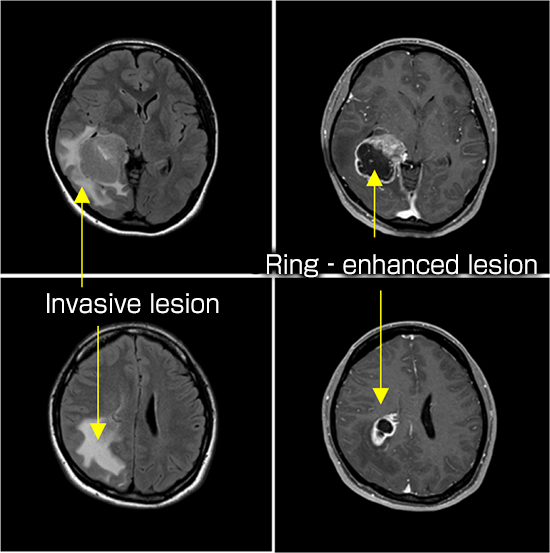
Wilson CB. Glioblastoma; the past, the present, and the future.
Clin Neurosurg 1992; 38: 32-48. 2